Today’s conversation between Griffin Jones, Dr. Milroy, Dr. Supogay, and Dr. Yanni explores the overlap between clinical operations and marketing. The fact of the matter is, you cannot totally separate them. More often than not, when our clients first come to us, they aren’t able to fit more patients into their system so we first have to work on clinical operation efficiency before driving more patients through the door.
In this episode we explore:
The REI bottleneck and how to optimize your REI’s time
Referral patterns from other professionals in your community
How patients choose an REI
Why OBGYN education improves the quality of patients
Inside Reproductive Health is sponsored by EngagedMD. For technology that educates your patients with true informed consent, visit engagedmd.com/IRH for 25% off your implementation fee.
Guests:
Dr. Milroy:
LinkedIn: http://linkedin.com/in/colleen-milroy-37a45ba1
Colleen Milroy, MD, FACOG is a board-certified Obstetrician gynecologist, and board certified Reproductive Endocrinologist and Infertility physician. She currently leads the Billings Clinic Reproductive Medicine group serving the state Montana, parts of Wyoming, North Dakota and South Dakota.
Dr. Supogay:
LinkedIn: http://linkedin.com/in/anna-sapugay-md-facog-66932714
Anna Sapugay, MD, FACOG is a board-certified obstetrician gynecologist who practices in Northern California's East Bay Area. She currently serves on the Compensation Committee, Strategic Oversight Committee and Anti-Racism Working Group. Sutter Health is a not-for-profit healthcare delivery system that operates 24 hospitals and over 200 clinics in Northern California.
Dr. Yanni:
LinkedIn: http://linkedin.com/in/leanne-yanni-md-9b6117194
Dr. Leanne Yanni serves as Vice President Medical Affairs, Richmond Market, Bon Secours Mercy Health and the Chief Medical Officer of St. Mary’s and Richmond Community Hospitals. She is board certified in both Internal Medicine and Hospice & Palliative Medicine.
Website:
Transcript
[00:00:55] Griffin Jones: On this show, it's half me interviewing my guests, half them, interviewing me. I'm not going to go into their intro and bio here because I do that a little bit in the beginning of the conversation, and then they introduced each other, but they're three different MDs in three different areas of medicine that are also in the MBA program at Harvard.
And. In today's show, we talk about OB GYN, referrals, OB GYN, relationships. There's some really good insights for you there. The show is really about where the nexus of clinic operations and marketing come together. There is a place after the overlap where I can't go any further and these three could, and there was a part where they wanted to go deeper in terms of using marketing to set up.
Client operations and I was able to go there. So I hope you enjoy this. This is the nexus of where the bottleneck of the REI field is addressed, where clinic operations and marketing come together.
Doctors Yanni, Sapugay and Milroy, Yanni, Anna Colleen, welcome to inside reproductive health. This is a little experiment that we're doing sort of on the fly. These are three MD MBA. Students at Harvard and Dr. Milroy, I know through the field of reproductive health and they are interviewing me about a project that they have.
If I can provide some insights, that's the reason you're listening to this podcast episode. And if you're not, it never made the light of day. You're my podcast editor throwing this episode in the garbage. So Dr. Yanni, Leanne, tell us a little bit about the team that you have and the venture, your.
[00:02:48] Dr. Yani: Excellent. So I'm Dr. Yanni and I'm an internal medicine doctor at Bon Secours Mercy Health in Richmond, Virginia. And we have my colleagues, Colleen Milroy, who is a fertility specialist in billings clinic in Montana. And Anna Sapugay who is an OB GYN at Sutter health in California. And we are all currently enrolled in Harvard, T.H. Chan school of public health, the master of healthcare management.
So very special, a masters it's focused on physicians. It's a two two-year program designed to support physician leaders and physician. We are currently taking a marketing class, taught by Linda McCracken. Who's very well known across the country for her marketing expertise. And our project is to define a clinical problem and a marketing strategy.
I'm using focused marketing techniques to address the clinical problem. And we have really chosen to focus on fertility and with Colleen. Expertise in billing Montana with her fertility expertise, we're going to focus in that area. So that's why we're talking to you today, Griffin, and really glad for the opportunity.
[00:03:54] Griffin Jones: The pleasure is entirely mine. Why did you choose fertility? Did Colleen strong arm, the rest of you? Or how did, how did you choose that? This was the opportunity in the nexus of medicine and business that we want to explore.
[00:04:11] Dr. Sapugay: So, you know, infertility, afflicts, not only insured patients or the wealthy, but it all, it afflicts all kinds of women in all walks of life and with expansion in billings. Our goal is to. Have health equity, even within the infertility sphere
so if we are able to reach patients with infertility issues in rural America minority women that would be something. That we would like to enter and possibly, you know, reach patients who have not been reached before in the infertility sphere.
So in your experience, what has been the best way to reach in for fertility patients?
Is it by engaging them directly? Engaging their community or going through the providers that they see, like their obstetrician gynecologist or their primary care physicians and for our target population. Would we do that differently for patients in rural America.
[00:05:28] Griffin Jones: So the second, the answer to the second question, would you do it differently is likely yes.
Because the answer to the first question is it depends on the area. There's effectively three different reasons. Why a patient selects a fertility provider. There's more, but three reasons make up more than 60% of patients. Number one reason above all of the others for choosing an REI the first is a referral from their physician.
That's 21% of patients say that that was their number one. Factor in influencing their decision referred by another physician. The second is referred by a friend at 20% and the third is location. At 19%. I could be mixing up two and three. I don't think I am. If I am I'll, I'll correct it in the show notes, but those three are on the heels of each other.
21%, 20%, 19% physician referred by. And location. I actually, I think location is number two. So I'll clarify that in the show notes, but they are all close to being on the heels of each other. This isn't to say that only 21% of fertility patients are referred by a physician or only 20 19% are referred by a friend.
It's just to say, that's what they say is the most influential in choosing their decision. So when you're asking this question, I tried to add a little bit more light on attribution and how attribution needs to be triangulated for fertility patients. We don't have a perfect CRM customer relationship management software that integrates with EMR perfectly.
That does not exist yet. Till we have that. And even when we do, we need to triangulate attribution, one way is volumes from whatever we're promoting. The second is in digital attribution, through a CRM, through Google analytics, through any other digital platforms that you have. And then third is patient self reporting.
And when you do the third patient self reporting, that is where you asked the question. Of the main ways that you're trying to reach patients, whether it's online reviews, social media, if you are spending a lot in traditional media, you would want to know, is somebody hearing us on the radio or seeing us on TV and the answers to those questions need to be binary?
Yes or no. There should not be more than eight of them. There should not be less than four. Then the exact number depends on exactly how heavily you're marketing in different areas, but they have to be binary. Yes or no. Last question is of all of the, of these ways of these four different. Four to eight ways.
What was the most influential in choosing your practice? And that's how we get to, to those numbers. So MD referrals are still extremely important, important. They're just not the lion's share that we sometimes think we are. And so I'll take a breather to let you ask any followup questions before we talk about what that means for Montana.
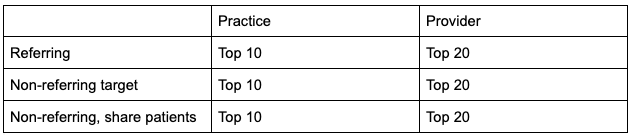
[00:08:49] Dr. Milroy: So Griffin, this is Colleen. We have been learning a lot about market segmentation, and you're saying you take the data from those sources, you collate it together and then use that to segment your market. Correct, and to different segments.
[00:09:04] Griffin Jones: You use it to prioritize your marketing efforts. So once you have a general baseline, which I've just given, then you also want to do it for your own.
You want to do it for your own patient base. So every practice should be doing should be triangulating attribution in this way for their own practices. And because those numbers might. Different. That's a net, that's a U S average that I just gave you. And so they will be different, but if you're so much lower and if you're finding that, wow, only 30% of our patients say they were referred by an MD.
That's an area where we probably want to invest more in physician outreach. And so getting that attribution one knows where helps you to know where you're going to prioritize. And then two, it helps you to see as you're investing in those priorities, what's being returned so that you can invest more in those areas.
[00:10:07] Dr. Sapugay: So Griffin, what I'm hearing is, so we have basically two target consumers, the physicians and then the patients themselves, when it comes to the am I right?
[00:10:20] Griffin Jones: Well, you, I, those are the two from the top, but you start to have more, as you start to have employers that have employer coverage. And so we've even started to expand.
Were you referred by, by your employer? Benefits broker did, did a progeny or a kind body or a carrot say. Well, here's who we've got on our network and, and this doctor's available. There's also apps in and lead generation and, and the friends themselves are a market in a way, but that could be a little bit tangential.
Let's just say you've got your, your, your, your top two patients physicians, and then a quickly emerging third, the employers and the employer benefit companies.
[00:11:02] Dr. Milroy: Okay, so I'll go up with the next stuff. So we have been learning and part of our project is to design something that has an improvement in the public health area. And so our question for you is clinical design solutions more important or is a growth solution more important.
[00:11:20] Griffin Jones: Can you define each, not just for the audience, but, but perhaps for me as well, if I'm being honest, I could guess what each of those mean, but I will help.
[00:11:39] Dr. Milroy: Yeah, a clinical design solution would be something that would improve either access or patient flow or things like that that would make the patient experience a little bit better or easier on the patient. A growth solution is where you're trying to right. Compete and grow in a market. And which one right now do you think is dominating our field in terms of being a.
You know a goal for fertility practices.
[00:12:08] Griffin Jones: This is very hard for me to answer. I feel that you're asking, which is more common place right now.
[00:12:16] Dr. Milroy: Yeah. What's the number one issue right now?
[00:12:19] Griffin Jones: Clinical operations is the bottleneck.
And so. That's partly inhibited growth. The experience that we have as a firm, when I came into this field, it was about new patient acquisition in some time in the past couple of years. Oh, let's call it 2018, 2019 we really had to. Away from that as a firm, because very few centers want for new patients.
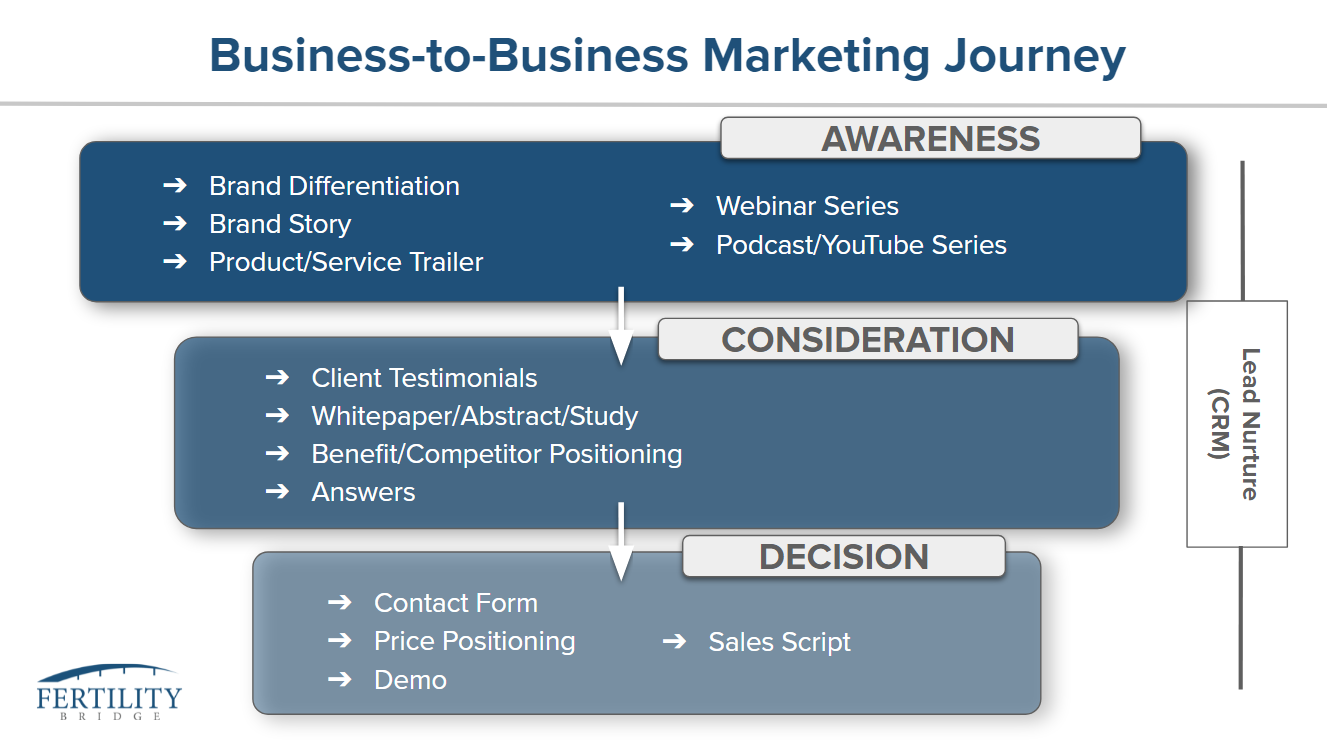
The bottleneck is on the clinical operational side. So as a business development firm and a creative firm where we've started to step in is in the third and fourth phase of the. Of the patient marketing journey at least the second phase and really only using the first phase to set people up, to move through the journey faster.
So not using content so much just to get someone in the door, but using content creative the way we answer the phone videos, digital. All to help people move through the journey faster and more easily. Take up less of clinician's time. Take up less of support staff time, not call support staff with. With redundant questions, not when they go see the financial counselor, they have some familiarity with what they're going to talk about, who the financial counselor is.
And so we have focused more on supporting, not, not supporting ops directly, but on the content that allows ops to operate more smoothly, as opposed to just getting new patients in the door. And so. I think that growth is inhibited by this bottleneck that we have in the field right now there's 1100 of you calling there's 1100 board certified REIs in the United States of America.
Give or take and of a population of 330 million people. And so. Things that I was hearing when I first entered the field in 2014, we would never use someone. That's not a board certified REI is one of our docs. Never. They have to be board server. We would never use a physician assistant. We'd never use a a nurse practitioner to help with retrievals, except they are now
and what was only a few people doing that a couple years ago now, very many people are, and the answer is because that bottleneck has to be solved for, and I would love for it to be solved for, because I would love to go back into super growth mode. But, but operations absolutely precedes growth as, as the need.
[00:15:03] Dr. Sapugay: Which is interesting question. Oh, go ahead.
[00:15:06] Dr. Milroy: No, I was just going to say out of 1100 board certified physicians, there are two in Montana that cover the entire state. So operations is going to be your bottleneck, right? There's only two of us, so that's a great, great influencer in our lives.
[00:15:21] Griffin Jones: And I don't believe that the two are, are mutually exclusive.
I don't think that they're divorced from each other when we're having this conversation. We have to choose then yes, I'm going to say operations, but the way I've built my entire firm is to support that operation so that, so we take what was growth in terms of acquisition and turn it into. Patients that have more, that are better educated that understand the process of the clinic that have rapport with the physician so that operations can move.
I don't think that they're totally divorced from each other. And I think. Too compartmentalized is a mistake, but to your point, Colleen, about there being two of those in Montana, that's the case in a lot of states and cities across the country. And I've talked about it a lot on the podcast that it concerns me.
I don't have data, but it just seems to me, if I talk to 10 fellows a year, eight of them are going to a handful of cities, right? It seems to me that 20 of the cities in the country are getting 80% of the fellows. I don't have data to support that, so it could be wrong, but it really seems that way to me.
And I would love to get that data for people. You know, it's interesting.
[00:16:34] Dr. Sapugay: You say that because we have alum, I'm the director of OB GYN in my department. And, and et cetera. And there's a long line of infertility specialists who are trying to present to my department of 34 clinicians. So there's a lot
[00:16:51] Griffin Jones: And tell us again where you are
[00:16:52] Dr. Sapugay: I am in the San Francisco Bay area.
[00:16:57] Griffin Jones: Yeah. And many of the people that have been on the show, including some of the fellows who have gone to the San Francisco Bay Area. So I do talk a lot on this show about what will become of your Buffalo new York's, where I'm from, or your Youngstown Ohio's or your billings Montana's.
And I try to make a. Plug that I think this there's actually a lot of opportunity for REIs and fertility centers in those areas, but that could be tangential to what you're looking into today. Or, or maybe it's not tell me more Colleen about what you're, what you're hoping to do, or at least exploring as a venture in these underserved areas.
[00:17:45] Dr. Milroy: I think so, one of the things that we're reading is something called blue oceans. It's a an evaluation in an article by Kim and Mauborgne and at the Harvard business review. And it talks about. You know, there are red ocean strategies that really are more in a competitive market that are driven by dog eat dog.
And then there are blue oceans and blue oceans are opportunities where companies, you know, really create long lasting, visionary, successfully evolving new markets. And so they're actually not competing necessarily. They're creating their own new pie. And so that's really what we're focusing in on is how do you create this new pie maybe?
And how do you serve a market that, you know, in a health equity, you know, access issue over the course of history has not really had an opportunity to visit us an easy way. So I'll let Anna kind of ask, cause I think, or, or Leanne had some questions about the actual products that we're thinking about.
[00:18:46] Dr. Yani: This is fascinating. And so one of the marketing questions that I have Griffin is you were referring to the advent of interdisciplinary expertise that is moving a little bit away from the physician as the sole owner of this type of. And, and really building up other expertise around our limited physician, which is our, our bottleneck as a marketer, how do you set the expectations of your population that you're marketing to?
That we do have interdisciplinary expertise and that is evolving. And, and while a physician may be at the helm of someone's care, there's a lot of steps along the patient experience that engage. Other clinicians and others with expertise that that can help them be successful
[00:19:31] Griffin Jones: Early and often is the answer to the expectation setting question.
And because we live in a world that is content dominated and we have yet to catch up to that as a field. That we live in a world that is content dominated every hour of many professionals day is dominated by the content they consume about what they're going to purchase, what they're going to eat for dinner, the research that they're doing for their work.
And using that to reset the expectations is necessary. Can't be the first time that someone calls on the phone. So, okay. So great Griffin we, we need to use content to set expectations about how it's thinking of content in the form of a Russian nesting doll. So if you think of all of the content on a topic, as deep as your point of view can go on something.
That's the, you might say that that's the. The tiniest hole doll within the Russian nesting doll and then an infographic or a shorter blog post, or a video might be the next level. And then a infographic might be the next shell. And then the next shell might be a Tik Tok representing the entire point of view.
And so when people are thinking of what's the best form of content that we should use as long form better is short form better. They both serve purposes and they both can lead to conversion both in form of acquisition and conversion to treatment. And they're both necessary for setting expectations.
But if you think of your point of view and start with. The point of view on any given topic. And in this case, we're talking about the support staff and including other doctors besides REIs and how they contribute to the comprehensive care being delivered. That point of view would start. I recommend starting as a really long article.
Really form that point of view. And then we create video from that. Then we create shorter. Then we create literally Instagram posts and then we create Tik TOK because they're all going to be seen by different people. And sometimes by the same people in that increases frequency, but we want people to. To receive these messages in different ways.
Some of them are going to some of them, it's just going to be straightforward. Some of them are going to be funnier and cuter, and that will depend on the brand voice of the people delivering the message. But to the extent that you're varying the content in this way, you can set the expectation with people that.
Don't have to always see the REI for everything. And I might be inferring into your question too much, Anne so tell me if I am, but I hear this from REI is very often that they think they equal the standard of the. Standard of care in patients eyes. And I don't think they universally equal the standard of care in patient eyes.
The bottom line is the patient has to feel and be cared for. The REI is a part of that. How much of a part of that will depend and needs to be experimented with, but. To the extent that we're setting people's expectations ahead of time that, Hey, you're going to see this person for this. Then this is John, your ultrasound technician, and this is Mary, your phlebotomist.
And this is Dr. Patel or this is your nurse practitioner to the extent that people are familiar with these folks ahead of time, it makes it a lot easier. That the REI doesn't have to be involved in every single thing all the time.
[00:23:23] This topic that we’re talking about today, the REI bottleneck access to care, the convergence of growth and improvement in clinical operations, is the perfect segway to introduce our new sponsor for the show, that I am so excited to announce to you. You know who it is? It’s EngagedMD. You know why I am so excited about this? Because of the 7 years that I have been in the field almost nothing has been so lopsidedly positive as the feedback that I've heard about EngagedMD. I have been recommending them for years, at least since 2015. I hear nothing but good things from the clients that use us that we recommend to use EngagedMd and from other people in the field and you’ve heard it too if you’ve listened to this show people come on this show there have been several episodes where people just bring up EngagedMd without me even asking. That’s why I had to go get a sponsorship from them. And I am so pleased to do it because this is a great time as you’re starting to think about you’re 2022. You’re sitting down, the investments that you're making to make life better for your staff and for your patients. The pretreatment education that EngagedMD allows you to scale, so that you have more rapport with your patients, so that you have true informed consent not just sticking a handful of papers or stack of papers and having them sign it but true informed consent. So that you can tailor the patient education that they need, the standard of care that they need. Talk to them about their diagnosis, their prognosis because they are better educated, they have true informed consent. That’s the type of scale that EngagedMd provides. More than half of our clients use it, I guess I gotta to talk to the remainder that don’t because everyone loves EngagedMD. And now that you’re planning for 2022, now is the time. It’s a quick win that you can give to your team to advance your practice because this is one of the leading companies in the field. They’ve got a product road map that’s as long as my arm, and they are going to be around for a long time. And you have the opportunity now to get a couple bucks off. Go to EngagedMd.com/IRH and you get 25% off your implementation fee. That's for new customers. If you're talking to them tell them you heard them on Inside Reproductive Health. Tell them you heard them from Griffin Jones. You get a couple bucks off with 25% off your implementation fee and you'll be starting your practice on the best start that you could have moving towards scale and moving towards patients who are better educated and have true informed consent with EngagedMd. EngagedMd.com/IRH. EngagedMd.com/IRH.
[00:26:14] Dr. Sapugay: So Griffin, going back to my question. Well, first of all, thank you for that.
But going back to my question of reaching our consumer, would it, from your experience, would it be different trying to reach rural America or specifically Montana where, you know, people. ARe four or five hours away that you're trying to reach.
[00:26:37] Griffin Jones: Probably, I can give you one thing that tends to be true for rural areas that is less true for
urban coastal areas, which is the readiness of how effective organic social media is. And I'm not talking about paid social media, running ads. I'm talking about organic social and the reach that comes from that I've known when ever we work with a small Midwest market group that. And I see they don't have much of a social media presence, but as long as I can tell, okay, these are good people.
Their patients are really happy with them that it's like taking a match to dry Tinder. And that doesn't tend to be the case in larger urban coastal areas. And my hypothesis is again, I could be wrong about this, but I think that it's because. In billings, Montana or Youngstown, Ohio, or Omaha, Nebraska, if you're 28 years old and you don't have children in many of those communities, you are not part of the social fabric.
And there's very few alternatives for you. And. The center in this case has the opportunity to stop and say, where do our community? You do have a community, you have lots of neighbors, and you actually know some of these people. We're not going to identify them, but we're going to be here. And as you start to identify yourselves, you'll, you'll start to, to perhaps talk to each other.
And now we, as the center are. At at this we, the IVF center at the center of this social community, that is a means, that's an advantage for rural centers that doesn't always exist for urban centers. And the good news for them is that it doesn't, you don't have to spend a lot of money on advertising necessarily.
You do have to spend the time to, to create the content.
Did that answer your question, Anna, what was that? Did I take that off the rails? No,
[00:28:52] Dr. Sapugay: it, it, it answered my question. Would you focus more on the providers then that are serving these patients and, and reach them through their providers? Because. As you said, if you're 28 and you don't have kids, you're sort of out of sync with social media.
[00:29:07] Griffin Jones: If I'm in a rural area, in a small market, I'm doing organic social first, the first thing I want to do is set up the attribution. So I know that if I'm wrong about this, but if I'm just having to pick something from the bat in a, in a rural small market, not even necessarily rural, but in a small market that tends to be a place where, where family is the social fabric and.
Not a Manhattan or a San Francisco, then it's, hasn't been the case every time or has it, I'm really trying to think almost every single time. It's the case that that what's missing is, is people knowing that my friend, my former coworker, my cousin. To all one went through this, but two went and saw this specialist that they're thrilled with.
And that tends to be the lowest hanging fruit in markets like this. It doesn't mean that physician outreach strategies necessary it very well may be. It tends to be the case in those marketplace that if, if, without digging into the attribution, which I would do, if I were actually talking to a client, if I'm just guessing, that's what I would do.
[00:30:21] Dr. Milroy: Chris. And I have a question. There's been an uptick into the direct consumer kind of fertility testing. And I just wonder if that is a way to reach the customer in a rural market or in a lower socioeconomic status or lower access, lower health equity area. Could that be a way that we connect with them
[00:30:45] Griffin Jones: first?
Well, I think anytime that you have to drive three. Plus hours to a physical location anytime. And for those of you listening, Colleen putting up or hands just up to eight hours in some of these, in the interior west, that can be the case. Yeah, these are absolutely areas that expand access that ultimately serve as lead generation for treatment and for centers.
So, you know, I've had. Afton Vechery the CEO of Modern Fertility on the podcast to talk about this concept. And some people might say, oh, that's not as good as the way we would do our testing here. And that may be the case. You can come on and debate it. I'm not a clinician. What I am saying is. It is a gateway into the next step.
And to the extent that we can take out testing from the office one, it serves as lead gen two. It improves access because people don't have to travel the distances. But third is, it goes back to tying in this theme of growth and this theme of client of clinic ops, where. It's triage for the clinics.
And in many ways, if you have a bottleneck of people a two month wait list of people trying to get in, well, wouldn't it be great if, if some of these people had more information coming into the practice and you were maybe able to refer out to some of those things that an OB GYN or even a PCP could do.
So I think triage is a part of. Of this, as well as bringing the themes of growth and clinic ops together.
[00:32:32] Dr. Milroy: Yeah, I, I wonder often, you know, in many of these kind of rural parts of America, the small critical access hospitals, many of them don't have the ability to run some of the tests. We would like them to run.
And so that direct to a patient's home where, you know, in the privacy of their home, when they don't have to go to this small town hospital where they know every single person who they walk, you know, walk by and really have to devulge this very private and scary, you know, diagnosis that, you know, they could be doing that in a little bit of a different way and putting it in the mail.
And I think that could be a really great way to, to access and to really, you know, care for these patients in the right way.
[00:33:16] Dr. Yani: I have one last question for me is do you think the future is directly working with payers and insurers to use this sort of home assessment kit in a way for fertility, for those who have a you know, basically ICD 10 diagnosis of.
[00:33:36] Griffin Jones: That's a great question. It might be above my pay grade.
Do you mean that the providers would, would require of the, the payers to, to, go through these at-home tests before. They sent the patient to the office.
[00:33:55] Dr. Yani: Well, so to give you an example payers are now acting in many ways, almost as a clinical conduit and a good example is, is colorectal cancer screening.
While you can't do home colonoscopy you can test your stool for blood or specialized tests to determine if you have a higher likelihood or higher risk of cancer. And so, you know, we can imagine a future state where someone has been officially diagnosed with infertility and context, their insurance company, and they're able to actually directly administer the tests.
I can imagine a future where then they direct them towards a fertility specialist that's in their network.
[00:34:34] Griffin Jones: I think this is part of the lead gen system that many of the tests themselves are trying to do. So you're bringing up something to me of that it's interesting of, of the employer benefit brokers being the insurance company.
Doing it and being a part of it, many of the, of these tests. And there are many of them, there's a couple leaders like the ones that we mentioned, but there's so many that are trying to get into the marketplace that are raising 10, 15. It's somewhere in the 10 to $25 million ballpark of funding. And part of this business model that they have in their minds is that they want to do exactly that well.
Okay. Well, here you go, Dr. Milroy, we have these patients for you. They're ready to go. We've screened them. And so far nobody's been terribly successful at that, partly because they've been looking at the. Provider to, to pay for that. And I don't think that that's the right model. I think anytime you can go around the providers, listen, I own a client services firm and we work with providers.
I'm telling you, it's not the best way to go. If, if you can get somebody else to pay for it, that's typically better. And so I can't speak to if for certain that I think that. Having the employer benefits and insurance companies providing for it, but it could solve the challenge that has come from the providers not, and I'm thinking of one company And they were pretty good at actually nurturing the patient and getting information.
And I don't remember to what extent they did a testing, but they actually received the money from the patient and they paid the clinic and they still couldn't make that business model work because the clinic fought them on attribution. So. I'm sorry that I don't have a, a great answer for you Anne other than here's where it hasn't worked on this side.
Maybe it could work on the insurance side and if it does attribution would have to be. Either not a part of it and because the insurance company doesn't care, they want to, they want to do triage and send less people to the expensive people first that they can. Or you know, that that attribution model makes sense for them.
[00:37:02] Dr. Yani: Yep. I think that's a great answer, Griffin and got us thinking about what is that blue ocean and how do we work out those bottlenecks and those issues to, to really expand this access for those who really, really need it.
[00:37:16] Dr. Milroy: Griffin, that's all we have for you. Do you have anything for us that you'd like to ask us?
[00:37:22] Griffin Jones: The question that, that I have is where do you see the provider involvement evolving in the next few years with regards to advanced providers with regards to OBGYN, what do you see happening in this area? Because if the bottleneck can open.
Bring a lot more water into the bottle right now, my firm is focused on, okay. We have a limited, we have a narrow passageway. We need to make sure that the what's going through that passageway is going through as quickly as it can, but I would love to open up the passageway. What do you see happening on the, the provider side?
[00:38:11] Dr. Sapugay: So I will have Colleen the last word, but as an OB GYN in my neck of the woods we actually do a lot of the initial work up and some of us do it all the way to, you know, our regular ultrasounds to look at follicles and then do intrauterine insemination. So we do do that, but it's also a very.
Saturated market in the Bay Area. And and so for some OBGYN who don't even do the workup, we have the REIs who will do it from scratch and, and take the patient all the way through.
[00:38:55] Griffin Jones: So I, as a marketer, that seems like the logical path to providing more access, getting more people in, but I'm not a clinician.
So I can't speak to that. Colleen play devil's advocate for a second. BV old, the old hawty REI that says only REIs can be doing this. What is the argument against having a non. Board certified, a non REI board certified OB GYN. Do the workup, do the IUI, maybe even do retrievals. If that's two arguments, you can break them into two.
But what was the argument against that?
[00:39:38] Dr. Milroy: So historically I would say it is training within that field enough that you feel comfortable really talking about the nuances and the side effects and the risks associated with things. I would say that's old school and I actually, Griffin, argue the other way, often where we are covering such a large geographical market we have to use position assistance.
So each physician is paired with a physician assistant. The physician assistant does the simple IUI, the ultrasounds, the simple infertility patients. PCOS patients. And then when those patients go through the process and they're getting to more of the difficult stages of things or surgical stages or IVF stages, that's when they're coming in to see me.
So I think it's operations and really who you train and how you train them. I think you know, we took a whole class, the three of us this summer on operations. And one of the things that we learned in that class that was super important to patient access and flow is what's called a complete. And so the way you optimize me as an REI is really to give me the patient tied up with a little ribbon and a perfect little package.
And so it's already to go. So that means I'm not ordering the basic test. It means I'm not ordering, you know, and then having them follow up with me to talk about a semen analysis, it's that all of that data. All of my team knows needs to be there before they see me is ready to go and perfectly ready for me to evaluate.
And then I can really use my degree to say, what do we do with this? What is the data out there telling me to do for next steps? You know, where is your highest chances? What's your quickest time to pregnancy. And so you're using my brain and that way, rather than ordering tests and so complete kits I think are super important.
We identified it in our operations project as one of the keys to really opening up access to fertility centers. Similar to,
[00:41:47] Griffin Jones: Well as a non-clinician I would love to see this. I would love to see the patients that are. Coming to the REI, the ones that are in most need of the REI, but there's a couple of things that I'd see sometimes.
And the only reason I'm seeing this, I was a D student in high school biology. So no clinical background I'm coming from just, I'm looking at referral patterns and how do we get people to move through the process more quickly? And sometimes I see people. That are coming to the stay at their OB GYN for far too long.
The OBGYNs doing time intercourse, they're doing IUIs. They're doing they might be doing some other things, but they haven't even tested the male partner for a semen analysis. And I'm like, oh right. Here's this other referral source. So. That gives me a glimpse into all right. That's probably a clinical oversight.
I'm not a doctor, but, so how do you create the framework that that is the right OBGYNs that are doing this, that they have. At least some training and maybe not an accreditation, but to get you what you need to have those patients with the bone. How does that happen,
[00:43:00] Dr. Milroy: Anna? And I can answer this together with her being a general OB GYN in the fact that I share
What I know as much as I can. And so when I go talk to the OBGYN when they are contacting me, I am sharing not only what we're doing, but why we're doing it. And so things like timed intercourse without a semen analysis probably not that helpful. And so right. Reminding my referral patterns where we live, it's not just OBGYNs, it's family practice doctors, it's critical access hospitals, it's nurse practitioners and physician's assistants that are actually really referring to me who really not never got training in this space.
And so it's really creating outreach for education for the, for my rural providers out there who may be see this three times a year. Right. And, and don't feel comfortable in that space. And so they're just trying to do whatever they can to help the patient. But in reality, they're wasting time. And so I think, you know, having access to me, like when they call me, we always answer them and always quickly respond.
And then spending time really educating them on what. What's really helpful for these patients. Anna, do you have another thought being an OB GYN?
[00:44:14] Dr. Sapugay: I was just going to say so basic infertility management is actually part of our training
[00:44:20] Dr. Milroy: for you as an OB GYN. Absolutely not for my physician assistant.
Who's at a rural access
[00:44:27] Dr. Sapugay: hospital and one of the things I cannot emphasize Colleen's point on education enough. So part of my condition, actually, whenever an REI presents to my department to try to get our referrals is to do some teaching to the entire department as part of their introduction. So educating clinicians, not just OBGYNs, but to Colleen's point, you know, primary care providers is key so that the patient's time is not wasted as they're getting worked up.
And, you know, one of the first things I always tell my patients who are coming to see me with infertility is men make up a huge proportion of infertility problems. And so that's actually one of the first things. People should be testing for and not always just assume that it's the woman's problem. The other thing though, that comes into the equation is insurance companies actually less when the OBGYNs or the primary care clinician does the testing, I suppose to when the the REI does the testing.
And so that's another reason people come to us first.
[00:45:41] Griffin Jones: Well, what you just described is why I don't think referring provider outreach is going away as a, as a strategy, as a business development strategy. It's not the end all be all of the single source of patient attribution, but it also ties into what's needed for triage to help qualify patients that are.
To the REI to move them through more quickly. So I've enjoyed this conversation with the three of you. It's having this clinical operations framework meet a marketing framework. They're not totally divorced from each other. It is a Venn diagram and they do overlap. So I do reach a point where I say this is as far as I can go on the train.
And and it's been nice to, to talk with the three of you of where those areas meet Dr. Yanni , Dr. Sapugay, Dr. Milroy, Leanne, Anna, Colleen, having three of you guests on, I wish you the best of luck in your MBA program. And thank you for doing that extra curricular business study to improve the quality of the standard of medicine and for coming on Inside Reproductive Health.
You’ve been listening to Inside Reproductive Health, sponsored by EngagedMD. For technology to streamline patient education and informed consent, visit EngagedMD.com/IRH for 25% off your implementation fee. That’s EngagedMd.com/IRH.