In this week’s episode of Inside Reproductive Health, Griffin Jones and Dr. Amanda Kallan debate the future of academic REI practices. They talk about the trade-offs as well as the positive future of academic practices. Being a Yale alumnus, Dr. Kallan is the perfect guest to share her view on the operation systems, marketing systems, and scope of practice an academic practice has versus private practice.
Dr. Kallen, MD, FACOG, is currently a reproductive endocrinologist at the Yale Fertility Center and an Associate Professor of Obstetrics and Gynecology at the Yale School of Medicine. Dr. Kallen runs an NIH-funded laboratory and has received multiple awards for research, including the Society for Reproductive Investigation “Early Career Investigator” Award for her work on mechanisms of reproductive aging. Her clinical interests include fertility preservation, access to fertility services for her LGBTQ patients, and primary ovarian insufficiency.
In this episode we cover:
Academic medicine practices’ shortcomings
How marketing blends into the standard of care
Distribution of funding for research
Operational differences of academic medicine practices (vs. private practice)
Dr. Amanda Kallan’s Information:
LinkedIn Handle
https://www.linkedin.com/in/amanda-kallen-58b80959
Twitter Handle
@AmandaKallen
Website URL:
Transcript
Griffin Jones: [00:00:40] On today's episode, I'm a little bit skeptical of the future of the academic REI practice, particularly because of their autonomy or lack thereof. This episode has a great champion though, in Dr. Amanda Kallen from Yale and we talk about her view on the trade-offs of academic practice and the positive picture that she sees for the future.
Before we get into today's episode today shout out, goes to Dr. Michael Hill thought of him because he's at Walter Reed. So this academic topic made me think of him I have no idea if Dr. Hill listens to inside reproductive health, but if you text him, then I might get a text from, and then I'll know today's episode who better to talk about the trade-offs of academic medicine and the positives than a true Yalie.
Dr. Amanda Kallen did her residency at Yale, she did her fellowship there. She's working there. Now she runs an NIH-funded laboratory. We talk about the sacred power of NIH funding, and she's received multiple awards for her research her clinical interests include fertility preservation, access to fertility services for transgender patients and primary ovarian insufficiency.
And we talk about some of those interests and how she's able to pursue them to the degree that she wants to in her practice because of the positive trade-offs that she used of academic REI practice. So you'll see me get into it a little bit with her making her defend it more than I have academic guests in the past, but she does a terrific job.
I hope I was fair. I'll let you decide, enjoy this episode of Inside Reproductive Health.
Dr. Kallen Amanda, welcome Inside Reproductive Health.
Dr. Amanda Kallen: [00:02:32] Thanks so much for having me. It's great to be here.
Griffin Jones: [00:02:34] There's someone I've known in my periphery profile, I have never actually known you, we've never actually met, I just remember you being one of the earliest people on my emails. And I don't remember all that happened to you.
Dr. Amanda Kallen: [00:02:46] I don’t and I, you know, I was, it was an honor to hear from you because I think, I guess I've been out of fellowship seven or eight years now, but I don't you know, and this is a new opportunity for me, so I don't know how we ended up on each other's radars. Well, I know how you ended up on my radar. I get your emails and I've listened to your podcast, but it's nice to be here.
Griffin Jones: [00:03:04] It's nice to have you. You're here representing academic REI in some ways. Omurtag, Bortoletto, Feinberg, and a few others. I will admit that it's one of the areas that I neglect. I'm more guilty of neglecting lab business than I am academics but I am pretty guilty with both.
So if there are people that are listening feel that I don't give academic REI a fair shake. You're more than welcome on the show. If you can give it some sort of angle to the rest of the show's themes. And one thing that I like to start with is just why academic. And there's a lot of younger doctors that listen, some going into academics some getting as far away from that as they possibly can.
What are the pros?
Dr. Amanda Kallen: [00:04:00] Yeah. So, you know, I think the pros are that you can kind of have your hands in a lot of different things. You know, the caveat for me is that I have only practiced academic medicine. I, like I said, I finished my fellowship in 2014. I joined Yale, which is where I did my fellowship.
So I'm a physician here now. So this is all I know. But that being said one of the things that drew me to pursue academic medicine and to stay was just that I kind of couldn't choose. I wanted to teach, I wanted to be able to continue research. I did bench research, some clinical research, but mostly bench research as a fellow.
And I really liked that it sort of fit I think a need for me to have some time to be sort of delving into a question, being very, hands-on doing my own thing at the bench and then returning to patient care for part of my days as well. And I didn't want to give that up. I had a wonderful mentor, who I could talk about sort encouraged that.
And then from the clinical standpoint, I really liked I loved infertility. That's one of the reasons I went into REI, but I also loved, I think the things that you, that people may see a little less of in private practice I started out with a really strong interest in pediatric and adolescent medicine.
And some of the things you see in that space you know, precocious and delayed puberty uterine anomalies. I did a rotation during my second year of fellowship at Cincinnati children's and I saw a lot of just really cool pediatric surgeries there. And that interest has kind of shifted a bit more to some other clinical interest as well.
But you know, I think being an academic medicine allowed me not to let go of any of those things that I wanted to do. And you know, it's you know, there's other challenges and sort of deciding that you want to do academic medicine and I think making the next step to finding a spot.
But it was really about sort of wanting to keep my hand a little bit in a bunch of different things. I think.
Griffin Jones: [00:05:53] How much control does one typically have over that, but in terms of their teaching responsibilities, their research responsibilities, their clinical time, how much is that? How are expectations for a set of what that is going to be if people have those interests that while they might be thinking they might be seeing, they might be spending 80% of their time versus how has that delineated?
Dr. Amanda Kallen: [00:06:21] Yeah. So, at least in my experience, I had a fair amount of, and I have continued to have a fair amount of flexibility in what I have focused my clinical practice on.
Know, I think all of my partners and I see infertility patients right now I have a particular interest in in seeing transgender patients and doing fertility preservation in the transgender population. And that's something that I've been able to really build on and focus my practice on a bit more.
And I've had full leeway to do that. So I think in, you know, and again, every practice is going to be different, but in terms of like the, just the pure clinical piece, like the kinds of patients I see in the work that I do, I've been able to really tailor my practice the way I want to, when it comes to like giving up your time, you know, if you look at a particular week How many days of that week, you're going to be seeing patients or how many days of that week you're going to be doing research or doing surgery or teaching?
I, that part, I think depends on more what else you're bringing to the table in terms of funding. So I have a lot of protected time to do research because I've been able to acquire a fair bit of grant funding, research funding over the last years. More in the last couple of years.
Griffin Jones: [00:07:30] Are you doing that grant writing yourself?
Dr. Amanda Kallen: [00:07:33] I am. I get a lot of I do a lot of sort of workshopping with people in terms of fine-tuning the grants, but the grant writing is coming from me and it's certainly a labor of love and sometimes just a labor.
Griffin Jones: [00:07:45] It sounds like a labor because it does. On one hand, it's like, well, you can, you're free to pursue different things in asterisks.
If you can get the funding and that isn't always easy to do, or I don't know the specifics of grant writing for REI research. What is it like?
Dr. Amanda Kallen: [00:08:06] Yeah, it's been so, you know, as someone who does basic science research, you know, so if I think back to how I kind of got started, what I had to do, you know, and I think a recommendation for people interested in like basic science research.
What I ended up doing was in my second year of fellowship, going into my third year, starting to apply for like training grants. There's different ways. Come out of fellowship with a pot of money that will protect some of your time, so that you can keep doing that research. And I ended up with one of those, is called the reproductive scientist development program.
And that gave me about five. It was five years of salary support so that I could actually protect about 75% of my time for research. And about 25% of my time was clinical and that's not, you know, every week isn't like that some weeks are more.
Griffin Jones: [00:09:02] Sounds like a big grant then.
Dr. Amanda Kallen: [00:09:02] Yeah. And that was the that's the intent of that particular grant it's specifically for like reproductive scientists.
OB-GYNs who don't necessarily have PhDs, but who want to do research that someone else might do, who came out with a PhD. And so that protected my time for about five years. And then there was a span of about two years where I really was cobbling together money from little grants here and there, wherever I could get it.
And you know, at some point my department has been incredibly supportive in terms of the hard jump to make from being a trainee to be, to having sort of independent grant funding. And it took me about seven years. But at some point, you know, having conversations with my department, they're like, listen, you're going to need to take on more clinical days.
If you don't have money to, you know, you got to pay for your time from somewhere. So I think it'd be from grants or from clinical time. And then at the time, the timing was such that kind of right around that time, a bigger independent grant RO1 came through. And so, so for me, I'm able to protect that time because.
Paying for it out of grants. Certainly, I think there are positions where a fellow might come out or someone might move and there might be some kind of like startup package or support for research or time for research, but the kind of the most guaranteed ways to, to pay for that time with funding.
Griffin Jones: [00:10:24] How common is it that physicians are securing their own grants? Is it also common? Maybe the division chief for someone else had secured grants and there's brands lined up coming from somewhere else within the university and a new doctor as an employee, not as a fellow being trained can walk into how common or not common is that relative to them securing their own grant funding.
Dr. Amanda Kallen: [00:10:52] Yeah, I think that's that's definitely something that happens and that's You know, I'd say probably that's a little more common. Because, you know, for example, I'm, I have my own funding, but I have a small stake on a couple of other grants where I do a little bit of work for people here and there.
And those I'm not the PI. Principal investigator, but I, you know, have my name on them and I participate them. And it certainly, I can think of other people in our department who have similar sort of roles in like bigger clinical projects, you know, patient recruitment, grant writing, that sort of thing.
So there's a lot of ways to be in an academic practice. There's a lot of ways to be involved in research that don't have to mean carving out this huge block of time to be standing at a bench. You know, doing basic science experiments, that's just one way to do it. But yeah, certainly to your point there, there can be ways to collaborate and get involved with other practices.
And I think that's really the way a lot of academic medicine and science is going is around sort of building these larger collaborations and working with other people because it is so hard to get money right now.
Griffin Jones: [00:12:00] I want to talk about that, but even, so that's one thread I want to go down. There's a second saying on this one is it.
Not even bringing in other people, but is it fairly common just to say, Hey, I have funding secured for this research, I'm not going to do it myself because I'm working on these projects. But you as the new employee, this is something you want to research. I've already gotten the funding is that common or does that not happen?
Dr. Amanda Kallen: [00:12:29] Yeah. And I would say that's very common and it could happen in a couple of ways. You know, one of one of the grants that I have, I wrote it that way and I designed it that way so that a collaborator who I work with gets a share of the money or doing a portion of the work that I don't have the time or the expertise to.
And that's, I think true of a lot of collaborative research. Like we, we can't all be experts in everything, but you can identify an expert and see if they'll collaborate with you and give them some of the funds to do that work.
Griffin Jones: [00:12:56] Those are the questions that a new doctor, academic job to be asking is these are my interests?
Is this BYO funding? Or question two might be, do you have what projects or research areas? Do you have funding allocated for?
Dr. Amanda Kallen: [00:13:15] For sure and I think, and again, cause it's can be hard to secure funding. I think I would go in, if I was interested in research, I would be asking what sort of projects can I get involved with that are ongoing?
What support is available for XYZ project that I'm interested in? What sort of support is there if I am working towards a grant, but don't have one yet? And then time, like what sort of time could be allocated to me to do that one? That would definitely, that would be a question that I would ask.
What kind of collaborative projects or what are people involved with already? That's collaborative and that's available for collaboration.
Griffin Jones: [00:13:52] So that's one thread that I want to go down is the collaboration with other entities and institutions. First, I want to dive a little bit deeper and build your practice the way you've wanted to mostly, can you talk more about what that means?
Dr. Amanda Kallen: [00:14:11] Yeah. So, you know, I think as a, you know, as a fellow starting out, I would see whatever anyone referred to me. And so my initial practice pattern was really a little bit of everything. I mean, You know, infertility you know, abnormal, uterine bleeding, uterine anomalies, septums endometriosis, fibroids, acne, you know, kind of a little bit of all sorts of things in both the infertility and kind of the endocrine surgery spheres.
And I think as I've practiced longer I've not only have I wanted to sort of narrow that down a little bit and try and kind of focus more on my own interests, but also I've had to because and this is one of the downsides of academic medicine. You know, if you think about, you know, 25% clinical practices about a day a week, obviously that bleeds into every day.
And I'm answering patient messages and calls every day. And surgery happens on other days and there's weeks where I'm on call I'm in the clinic every single day. But when a patient calls up to book with me she will be offered one, the one day that I'm seeing patients and that books out a fair amount, because it's more limited availability than my partners.
And so I really have had to start to narrow down kind of into like a niche-specific things that I want to do. So I think that I'm fortunate in that the practice has allowed me to do that and then supportive of that. But if I think just in terms of the volume and like the wait times we would've had to do it anyway, you know, I would need to do something like either stop seeing new patients or sort of limit the kind of new patients I see because at some point, you know, it's a balance between, you know, you're trying to do everything. But you want to do the things that you do well, and you want to provide your best care to patients too. And I think that is starting to involve kind of limiting the scope of practice a little bit.
Griffin Jones: [00:16:11] So you've been able to build more practice, mostly in clinical focus. But what about operations, because this is where I get really skeptical. When people tell me, then they'll say it on the show and they're great academic docs and say 'sure' you know, we just have to get approval and we need to go through this.
This is not what I'm seeing happening in the real world. So talk a little bit about operations and when you want to make operational changes you may be communications or image changes or HR types of changes within your organization. Talk about that a little bit.
Dr. Amanda Kallen: [00:16:55] Yeah. I think what you know, I would agree with what you probably have heard from, you know, others that it, Um, I have less control over those things. And I think, you know, I was listening to your podcast with Eve Feinberg at some point recently and sort of how she was describing like how control changed from a private practice to the academic model and kind of working in a bigger hospital system and how that control changed.
And I have had the same experiences, some of the changes I can make, you know, I can just tell someone, you know it, for example, I basically said I'm going to start limiting my patients. The justification is that my first new patient visit is the end of September.
And that, I think there was no sort of pushback with that big, bigger things do happen. And I think you've used these words more by committee or more at a sort of level above my pay grade. So, you know, staffing changes. You know, I don't necessarily involve my input marketing doesn't necessarily you or I should say I have input in those things, or I can voice an opinion in those things, but those are not decisions that are made by me.
And in some ways, it's nice to not have those responsibilities. But certainly, I think for someone like me who like to have a lot of control. There are some areas where I have a lot of control and somewhere I I have a little bit less and I think that's the nature of, you know, again, I don't have a private practice background to compare it to, but I think that is going to be the nature of working in a hospital system.
Or an academic medicine system, is there many more sort of stakeholders or decision-makers beyond you know, beyond yourself and I think that's part of why I like to have my research and teaching hats so much is that, you know, I can do my patient care. I do it in the you know, in the sort of within the constraints of academic medicine, but the pros and cons that go with that. And then when I put on my research hat, I am in full control of that, you know, I decide when I want to get up and start writing, I decide where I want to write. I decide if I want to come to the office or if I want to write in a coffee shop that day, you know when we're having lab meetings.
So, it is a nice balance in terms of feeling like I have control over a lot of the things that I do.
Griffin Jones: [00:21:47] That's what I wanted to ask you some more about is that trade-offs, it's clearly a trade-off and I want, see what's valuable enough to what type of physician profile to accept the trade-off of the lack of control in certain areas.
Because when you're talking about different departments and committees, It's already driving me nuts just from what I learned from you in our 5 minute conversation, but I'm the principal of my company. So I have a proclivity towards a certain way that isn't for everyone. You talk a little bit more about the trade-off
what is worth to you, I guess to say, you know, what, if I don't have controls over these areas, that's okay. Because I'm getting a, B and C more about those.
Dr. Amanda Kallen: [00:22:36] Yeah, I think I would imagine that in every sort of practice model, there is some relinquish relinquishing of control somewhere. And so in my practice model where I relinquish some control in terms of those bigger decisions that might be made, you know, in with us as a group or, you know, at the level of the administration where I have pretty much full control is in, you know, what kind of patients I see the breadth of patients. I see now, which I don't think is necessarily going to be true in a private model that's more infertility-based.
How many well, I should say how, whether or not the type of patients I see, bring in a lot of revenue. You know, so I don't have to worry if I want to build a practice around transgender medicine or pediatric adolescent medicine, as it relates to REI or fertility preservation, I don't have to worry about it.
You know, how much money that's going to bring in for the practice. I mean, I don't want to say I don't have to worry about it at all, but it's much less of a consideration. So I really do feel like if I want to fit in a particular patient, I can do that. You know, if it's especially if it's something that interests me and I can provide that service for the patient.
And then I think, you know, think, you when you said, you know, liking to sort of be in charge and, you know, having control, I think I'm the, you know, I'm in my lab, I'm the CEO. I, you know, I run the show, I have absolute and total control in that space. And so I think that balance is kind of the clinical piece of things.
The other way, I would say I have a lot of control is just in terms of flexibility. So I can, you know, on the days I'm seeing patients are fairly set, you know, I alternate Mondays and Wednesdays in two different locations. But my other days are really mine to structure. And that could be coming in and, you know, taking my lab through some experiments today.
It could be, you know, especially during the height of the pandemic, writing a lot from home writing from the parking lot at my kid's school, if I have a few minutes, you know, it, there a lot of the work there's a lot of flexibility and not all of the work, but a lot of the work there's a lot of flexibility in both where I do it and the times in which I do it, which for me, I really like, you know, I have a family, I have a five and a half year old son and to be able to.
I'm also a really early bird, but I'll get up at five. I'll write for a while. I'll work on a grant or a paper. I'll think they can just Google. Then I'll come into the lab. And and I'm able to kind of structure my day around things that are important to me, but also get those things done. Clinic days are obviously less flexible.
I'm coming in and starting at a certain time and finishing at a certain time. But that's a real plus for me. I really. I liked being able to do that.
Griffin Jones: [00:25:29] I think a study on the sleep chronotypes of REIs would be interesting because my guess would be that many of you over-index for that early bird profile? There's probably a couple of night owl REIs. I feel bad for them, you've given us a good picture of the trade-offs of what you're getting and where you're not getting and that's I think that is. A good framework tab going into any position because in society there's a big emphasis on entrepreneurship right now.
It's just, it's not so glamorous. It's not all of the Instagram stuff. I get a lot, but I also give up a lot. And when I'm rooting for people, I try to be very specific about the roles of their seats, because I try to recruit intrepreneurial people. These are people that don't want to deal with the HR. They don't want to deal with taxes or insurance or government or that those levels of responsibility of owning a business and, but they want to own creative. Let's say they want to own digital strategy and those are the people that I look for and it sounds like you were able to strike that trade-off before I move on to the next mini subject, was that explicit when you were moving into this job or interviewing for it or applying for it?
I know you did your fellowship there, so maybe it was a bit more, just came out during your training, but how much of that was explicit as you were pursuing this job?
Dr. Amanda Kallen: [00:27:07] You mean in terms of the, just like, how, like how's the day would be structured or how much would be like yeah. Yeah. It was, I would say it, I knew it was explicit before I started the position because I, you know, I started sort of, I was fortunate and that I was coming out of fellowship with some grant funding and that grant funding mechanism actually specified she has to have X amount of protected time. So that made it really easy\ without that it would have been much more of a negotiation, you know, happy, you know, we cannot, you know, if I was going to a different place, we can offer you 50% protected time for research and 50% clinical or something like that.
And I do think in most places you would leaving fellowship and going into an academic practice or staying. You would want to start with that explicit sort of discussion about what can be offered in terms of protected time? I think what was nebulous for me was that that was always going to change depending on,
where the grant money came from. You know, so I had that time of that timeframe of five years that I had that protection. And then after that, it was, are you going to get any more grants or not? And if you don't how are you gonna pay for your time? And it's going to be seeing more patients. And so, but yeah, I think for me it was fairly clear what things would, it was fairly clear what things would look like initially and then sort of nebulous. I mean, I remember thinking in a sort of panicky way, like three or four years out, like, I don't know what two years from now is going to look like, because I have no idea if something else is gonna come through or not. So that part is can be scary. But initially it was pretty clear.
Griffin Jones: [00:28:46] Okay. I want to start to explore the future of the academic REI practice. I have a feeling that the top of the control is going to come back within that context, but I am curious about what you think is going to happen with these partnerships, these purchases that starting to happen because I don't know that I can speak on this definitively enough.
It's just what I'm starting to see, which is, I feel like this new wave of private equity consolidation and network groups or network partnerships, whichever nomenclature, someone prefers is finishing off the job. That the private docs started 25 or so years ago in taking some of these REI divisions or at least, you know, the IVF practice out of it or moving in, but it's their umbrella in the university's room.
Talk about what you see happening there, or if you can't speculate what you are starting to observe with that.
Dr. Amanda Kallen: [00:30:01] That's a great question. You know, I think for someone, you know, like for someone who's in my position who has some protection through funding for research, wherever that comes from, I think that'll continue. You know, I think that. There's always going to be this sort of tension and, you know, this exists even in my practice now.
And I think everywhere when, or as an academic physician or physician-scientist there's always this sort of tension of, should I be doing more research? Should I be seeing more patients and, you know, and how do I split my time? And, you know, when things get busy, when COVID happens and volume, you know, for us volume dropped obviously, but then picked quite up a bit after, you know, should I be giving up some of this time to be doing more clinical?
Should I be taking call? I take the same amount of calls my partners. And so I think that I think some of that tension will be. Will be sort of resolved or kind of depends on where that, where the protection for that time is coming from. I would imagine. And again, this is just purely speculation.
I would imagine that as practices change if someone doesn't, you know, I the amount of time that an academic practice might be able to give to a physician-scientist or an academic physician to, to devote to. You know, thought work and grant writing and things like that might change unless that time is protected by a funding mechanism.
I'm not quite sure if I'm making sense.
Griffin Jones: [00:31:43] What about how those funding mechanisms would work in such partnerships, like would these institutions issue grants to institutions that are either owned entirely or partly owned by entities that are profit-generating organizations?
Dr. Amanda Kallen: [00:32:03] Yeah, I don't know. I know that, you know, I'm thinking of a colleague of mine who has a practice model where she part of her employment comes from a medical school, an academic center, and that portion of her time is her time to do research is her time to do teaching is her time to build the sort of the academic pizza's the REI practice.
And then half of her time is paid for by a private practice where she does that work. And so I could see very easily things turning into something like a practice that was maybe absorbed, where there was an academic focus, maybe turning into something more like that, where there is still time available to devote.
You know, academic medicine because places need fellowships. You know, we need academic REIs. I don't think that'll go away, but maybe.
Griffin Jones: [00:32:51] But I think that's why it's going to happen. What's the hardest thing for most IVF centers right now is recruiting doctors. We had, this is not a private conversation, we had Mark Segal with US Fertility and he speculated that they might get 14 of the 44 fellows for. Partnership or four groups like that's hard to compete with. And so if you're one of the larger groups, you have the opportunity to purchase, at least the, maybe not the REI division, but you're buying the IVF center and you're starting a fellowship program through their work or now your fellowship program is joint with the academic center. And it's certainly not everything from a recruiting standpoint, not everyone goes to where they did their fellowship. Even if it is a, they have the private or the public, excuse me, the academic route to go either. But but it is an advantage and I think that's my speculation that we're going to see more of that.
Dr. Amanda Kallen: [00:34:00] Yeah, you know, and in my experience, I have not seen, you know, you sort of asked the question of like, will funders want to give money to people practicing in that model, that sort of split model. And I haven't seen that's a consideration like I, you know, and I've read a bunch of grants at this point, and I have never been asked to account, except for maybe on training grants.
I've never been asked to account for how my time is spent when I'm not doing research. What I've been asked to account for is? What have I produced? And what are the resources behind me? So, you know, I have Yale behind me and all of the resources that, you know, Yale can provide and who are my collaborators, know, that's a big piece of it is who are you collaborating with? What expertise do they bring to the table if you're junior? And I haven't, had to sort of defend, you know, well, I do see patients 25% of the time our practices changing, or it's not, or we're seeing more patients because of COVID-19 COVID is kind of presented a different situation because everyone's research, practice patterns have changed but I think as long as somebody can buy has, or confined the time to get the work done, either by him or herself or in a collaboration, I don't think funders are looking at what are you doing with the rest of your time, as long as you're productive with the time you have and that kind of brings me back to the, you know, what I think is one of the pros or cons, depending on how you look at it of like being in a field or a practice model, like this is I just have to produce, and it doesn't matter,
how or when, or where I do it, I just have to show at the end of a funding year that I've gotten the things done that I said I would do. And so I think when they're deciding, you know, when there's not going to be more funding, they're basing it on did I get done the things I said I would do? It doesn't matter if it's four in the morning when you know, up as an early bird or on a weekend or on vacation, as long as I get those things done.
So I know I sorta took us tangential a little bit, but I think.
Griffin Jones: [00:36:04] Well, I'm with you there. And if I'm being speculative and playing devil's advocate for private or large groups, partnering, buying part of academic divisions, I suspect they would say maybe they even said it on the show and I don’t remember; that they can be grant funders as well.
So they can then contribute from their profits to the research of the Institute.
Dr. Amanda Kallen: [00:36:31] For sure. And that, I think that speaks to the fact that we are having to be more creative and unique in the ways that we get money, because sort of the, I think the classical or traditional ways of getting funding, you know, you think like in an academic, as an academic physician scientists and the sort of holy grail is to get an NIH RO1 and show that you have this like independent funding, but that's, you know, those are harder and harder to come by.
And that's not the way that a lot of people are getting funded. A lot of people are getting funded through, you know, private grants, you know, through companies or groups, funding their own research. Exactly as you said so, yeah, I think, and I think that's kind of a plus of, I think that's, can only be a good thing is, you know, having more money available to ask and pursue these research questions, wherever it comes from.
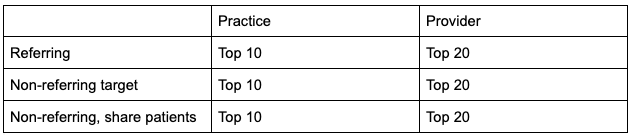
Griffin Jones: [00:37:24] Let's talk a little bit about the future in the sense of control as it is now because I really see some institutions having their hands tied behind their backs. And when I started in the fieldset seven years ago, I think it was really just marketing was really just bringing new patients in but over the years, since people have been coming so busy, it's less about bringing new patients in most centers don't new patients in the door, but it, the same things that we used to bring new patients in the door are now used to reeducate patients are used to help them align with self-select, what they want out of a provider to educate them on the process ahead of time.
So that they're not calling the nurse all the time to reset expectations because they're coming in with Uber, Instacart, Airbnb type of expectations or Amazon expectations where everything's instant. So the same things, the same channels and content and styling that we used to do to bring people in the door we're now using to help people.
Self-select better be more educated, have more rapport with their physician and make that process easier on them, easier on the practice and I'm just like I'm seeing academic centers catch up with 2015. Right now, Amanda, congratulations you guys finally got Instagram! Already on the next thing. And so, I even sorry to put Yale on blast, that website looks like it's 2010 and because it's in Yale's website is not you probably I'm making an assumption that you guys can't have your own. So like, I just see the, what I've talked about for the past couple years is what starts off as marketing often just becomes part of the standard of care. It's how you communicate with people. It's the values you stand for, it's how you galvanize your team.
And so I don't know, that's kind of a rant. I don't know if it's a question, but love to comment.
Dr. Amanda Kallen: [00:39:46] I would agree with everything you've said about sort of how marketing is different in a larger academic center. I think it's funny. I had a patient a few months ago, come in and, know, said I'm all over Instagram and you are, Instagram is terrible. It needs a lot of love and I think you're right.
Like we I think something I'm envious of and also I'm happy to have no part of is how intense sort of the marketing has to be in private practice or often is in private practice. You know, I see my counterparts doing this amazing outreach on Instagram and Tik TOK and videos and all of those things.
And we don't do that to that degree. I think some people do individually but a lot of that does have to come from Yale rather than, you know, us, I mean, I could do my own thing. But it does of happen at a different level.
Griffin Jones: [00:40:47] They don't have to do that for marketing to bring in new patients anymore.
Maybe they did six years ago. I think they, prior to that, that they did have to do it to meet those volumes. They don't need to do it for that reason, but now they can do that. And these people will tell you that their patients listen better. They ask better questions. And as one of them has said, it's partly because you're otherwise, it's such a one-way street.
Someone's coming into your office and they're telling you how everything and they're telling you everything about themselves and they know nothing about you and this balances that a little bit, and it also helps to reset expectations important and I just don't see, I don't see academic centers catching up as quickly because they're used to not marketing, but now that we're beyond marketing, they're still behind.
Dr. Amanda Kallen: [00:41:48] Yeah. And I guess, you know, my way of sort of dealing with, or coping with that is, has become on an individual patient to patient basis. I think I can't you're right. The marketing is not something that I have a lot of direct input in. And so I don't necessarily have a lot of control over how the patient hears about me if it's through. And I know what we're talking about, both new and return patients or how the patient hears back from me. We've got this patient portal you know, the hear back from our nurses, our MAs, but I think what I try to do is deliver that in the visit, I mean, I'm, you know, when I'm seeing a patient I'm and this is true, I think of all docs, but I'm pretty transparent about, you know, myself and my own experiences, you know?
I have a patient who's having a miscarriage. I will share that I have had two, and, you know, and really try and sort of be an open book in terms of that back and forth. So that even if they're not getting it from me through social media, that at least they are feeling like they're getting that from me in the visit.
I think that whenever you have a practice, like ours is structured. The other thing you need is a much better infrastructure slash dedication to keeping those lines of communication open because you know, and I talked about this before, but the other piece is just that the patients can always get ahold of me because there are days when I'm in, in lab and not seeing patients, or it can be hard to get back in for a return visit.
And then that gets frustrating. So I think trying to do as much as I can in the visit to make that to build that connection and then make sure that the frontline people who are working with my patients, the medical assistants, the nurses, the staff to make sure that the patients feel like they have an open line of communication with me, even if there are some intermediary steps along the way, if that makes sense.
Griffin Jones: [00:43:46] It does make sense and at risk of this belief, belaboring, this point listeners are by like, perfect move on. I'm stuck on this because I think I can thread the needle here. It's the constraint that you're talking about. I have no doubt that you do everything you can to maximize that you have with someone when they're face to face with you, that you are authentic.
I've only known you for an hour at this level, I get that from you. And I don't doubt it for a second. You have that constraint versus other people that they have the same time and they have other mechanisms to leverage that time because we know how so many patients meet a doctor for the first time they come to the clinic for the first time they're a deer in headlights and they can absorb maybe 15% of whatever the interaction involves and this podcast that you're on right now, all of the content that we create about all of our systems about all of our processes is all pretty much for one purpose, which is that when people want to do business, that they actually show up and can receive what I'm telling them and share about themselves.
And they're willing to do that because they've listened to a hundred podcast episodes that listened to my book. They at that point, they're ready to say, okay, we're ready to share with this guy. And then I can get what I need, which is just a fricking business objective all of this whole operation is just so that people will come to me and give me an honest business objective that I can say yes, we can do that.
Or no, we can't purchase like this dance. And I know that it's not the same with patients in terms of skepticism necessarily. But often it's just that like that deer in headlights impact. And if academic centers aren't able to just create content everywhere and do it in creative ways and fun ways and novel ways, then I just see other groups.
Or other physicians at a big advantage for how they're able to treat patients.
Dr. Amanda Kallen: [00:46:07] Yeah. And I think I completely agree with what you're saying. I would like to see our content creation or marketing. Be even more ahead than what it is, I have seen a big push in the last couple of years in terms of doing that, it's still on our, you know, it's on our website.
You know, you can argue that needs some love, but I do think there is a lot more attention than there used to be to that and I think at the end of the day, patients will, you know, they'll look for the provider, that's the right fit and if the provider that's the right fit or the doc that's the right fit is the one who has that active presence or that really up-to-date content.
And then they're not necessarily going to come to me. You know, if it's a patient who likes the write-up about me or has, or, you know, I think, and this is really more the case for like my type of practice is word of mouth or referrals. You know, I'm a private OB-GYN, we'll have a patient who maybe has had a good experience and they'll say, go see Dr. Kallen, you know, she has an atrocious list. But you know, give it a shot and that's, I think often, you know, maybe the kind of patient that will end up in my office is a certain kind of patient who maybe doesn't place more value on some other things than the social media piece. And I'm not saying that's not important, it's critically important.
You know, if we're not sort of doing it at the same level that some of the private practices are we do what we can with what we have.
Griffin Jones: [00:47:47] Well, I'm going to give you the final thought of that. I'm going to be slight, I'm trying, I'm going to try to not be so self-serving I think a good lift for this task for academics started listening is if you were allowed to do our goal diagnostic I know that most academic centers will not be able to move on to the education phase with us. I think that's totally fine, but if they can't swipe a credit card for $600 and sit with their principals of their division to talk about some of these things too, at the very least get attention from their center and that they will get that if they do that and they bring that to their health systems.
They might not go with us after that very likely they won't, but they'll at least get some attention from those people. They will perk up if somebody else is looking at their stuff making a couple of suggestions. And so the litmus test is if they can't do that then I think that is really just a site, one lack of autonomy.
But I do want to give you the final thought and you can wrap the bow on it, however, you want if you want to give one to rebut that idea on control if you just want to talk about the future of what you think academics, REI practice will hold or advice to those entering it. I give you the stage.
Dr. Amanda Kallen: [00:49:14] Yeah, I think I guess I would just sort of wrap or circle back to kind of, I mean, I think that you know, the the issue of control as kind of come up in different ways through this interview, I think,I guess my take home would be, you know, well, I think like any practice, there are some areas, you know, in the past that I've chosen like academic REI.
There are some areas where you have a lot of control. And somewhere you don't and I think it ends up being that some of the areas where I have less control are also less of my time, you know so if I bristle a little at lack of control in some areas at the end of the day, I am seeing patients for this portion of my week.
The rest of my week, I have a lot of control and I have control over, you know, even a fair number of things, you know, my clinical day-to-day practice. And so I think it's I think at the end of the day, it's all about just kind of perception. And if, you know, Where you would like to sort of have the most autonomy because none of us are gonna, I mean, none of us not, that's not true.
Many of us coming out of fellowship may not have it in every aspect of our day-to-day practice. So it's just where you get more of it and I think where you get less of it. And then if that aligns with your goals for how you see yourself practicing for me coming out of fellowship into an academic practice very much aligned with what I was looking for from day today.
Griffin Jones: [00:50:45] And you've had to defend, or at least expound those trade-offs in this interview more than many academic REIs who have been on the show. Probably because I noodle on something after a conversation. I want to dig more into that, or I don't think stuff gets the front of it so you've done a very articulate and compassionate job of explaining and perhaps promoting those tradeoffs, Dr. Amanda Kallen, it's been wonderful to have you on.
Dr. Amanda Kallen: [00:51:20] Thank you. It's been really nice being here. I appreciate the conversation.